- University of Kent
- Biosciences at Kent
- People
- Professor Martin Michaelis
Professor Martin Michaelis
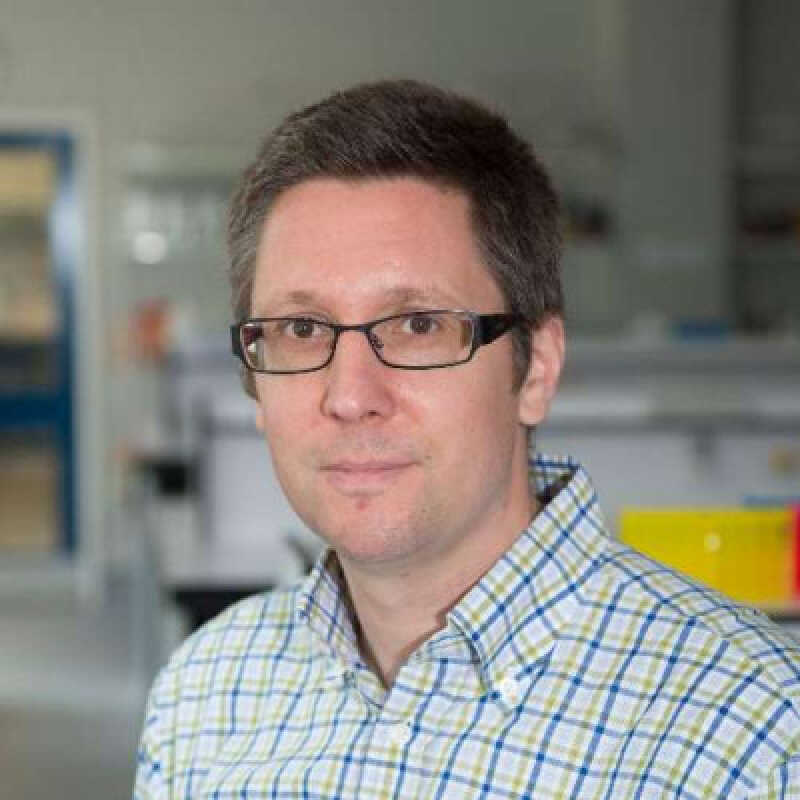
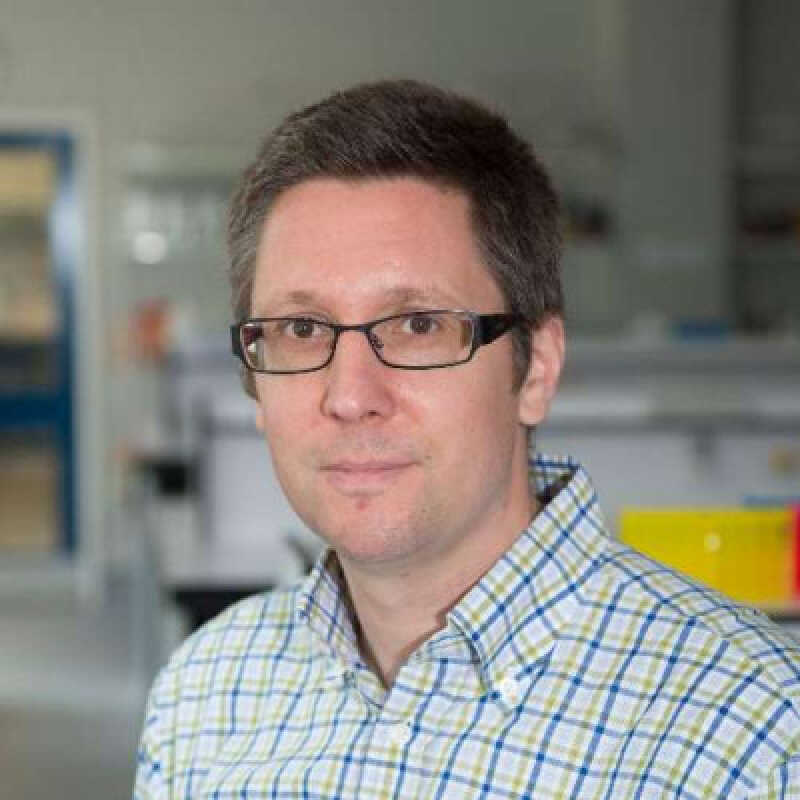
Martin Michaelis received his Pharmacy Degree (Approbation, 1998) and his PhD (2001) from the Goethe-University, Frankfurt am Main, Germany. He then worked as postdoc and later deputy group leader in the research group of Professor Jindrich Cinatl at the Institute of Medical Virology (Goethe-University, Frankfurt am Main, Germany) and the Dr Petra Joh-Forschungshaus, a private research institute run by the Frankfurter Stiftung für krebskranke Kinder in Frankfurt am Main. In 2011, Martin joined the University of Kent. He runs a joint wet/dry laboratory research group together with Dr Mark Wass.
Martin’s recent work has focused on Covid-19, and he has provided expert media commentary on vaccines and other treatments, variants and restrictions. His expertise on Covid-19 has seen him feature in a range of news outlets including The Daily Express, The Daily Mail, BBC Radio Kent, Daily Mirror and The Sunday Telegraph.
Professor Michaelis' research is focused on the identification and investigation of drugs and their mechanisms of action. The primary interest lies on acquired drug resistance in cancer. In collaboration with Professor Jindrich Cinatl (Goethe-University, Frankfurt am Main), he manages and develops the Resistant Cancer Cell Line (RCCL) Collection a unique collection of >1,300 cancer cell lines with acquired resistance to anti-cancer drugs.
In addition, he is interested in virulence mechanisms and therapeutic targets in viruses and in meta-research that investigates research practices in the life sciences.
Loading publications...
Showing of total publications in the Kent Academic Repository. View all publications